Introduction
This analytical report is the third milestone of the European Cancer Inequalities Registry, prepared in collaboration with the OECD. It is the first of a cycle of analytical reports and builds on the 2023 EU Country Cancer Profiles.
The report addresses the latest trends in cancer incidence and mortality in the EU and reviews key cancer risk factors, cancer screening programmes and early diagnoses. It examines policies and actions to tackle cancer across the EU27, Norway and Iceland, with a specific focus on addressing preventable risk factors and improving the reach of screening and early diagnosis to counter disconcerting cancer trends and inequalities.
Country performance, cross-cutting challenges and new developments are examined with a particular focus on disparities by regions, socio-economic status and gender.
Key messages
Cancer causes almost a quarter of all deaths in the EU27, Norway and Iceland, with five new cancer cases diagnosed every minute in 2022. While cancer mortality rates decreased by 10% between 2010 and 2020 in the EU27, wide variation in cancer outcomes exist across countries and even within regions.
Cancer mortality rates vary 1.6 fold across countries, and by up to 37% between regions within a country.
Age standardised cancer mortality rate (ASMR) per 100 000 population
by NUTS2 regions
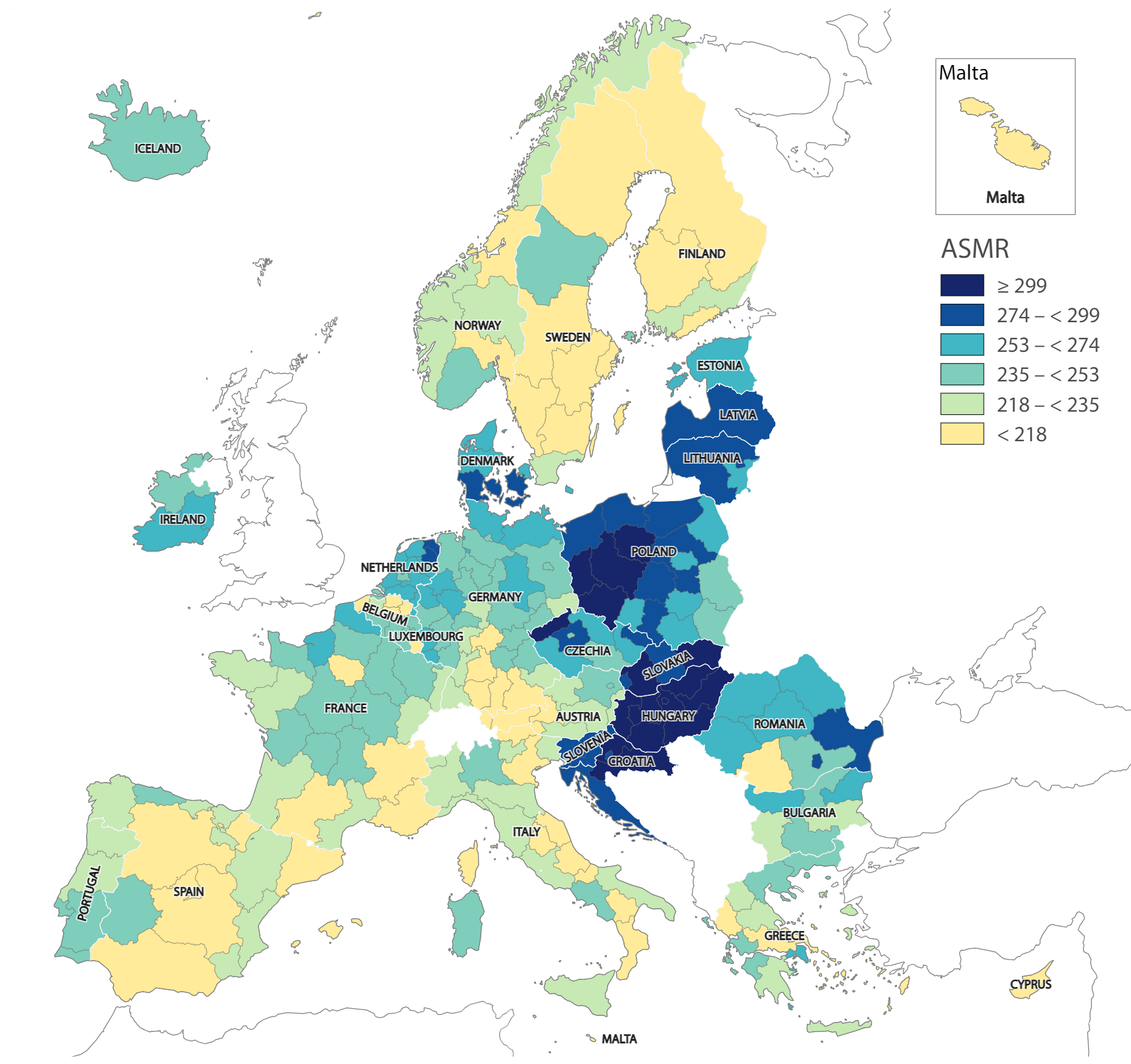
Administrative boundaries: ©EuroGraphics ©UN-FAO ©Turkstat
Cartography: Eurostat - IMAGE, 12/2023
Source: Eurostat (2023), Causes of Death – Standardised Death Rate by NUTS 2 Region of Residence.
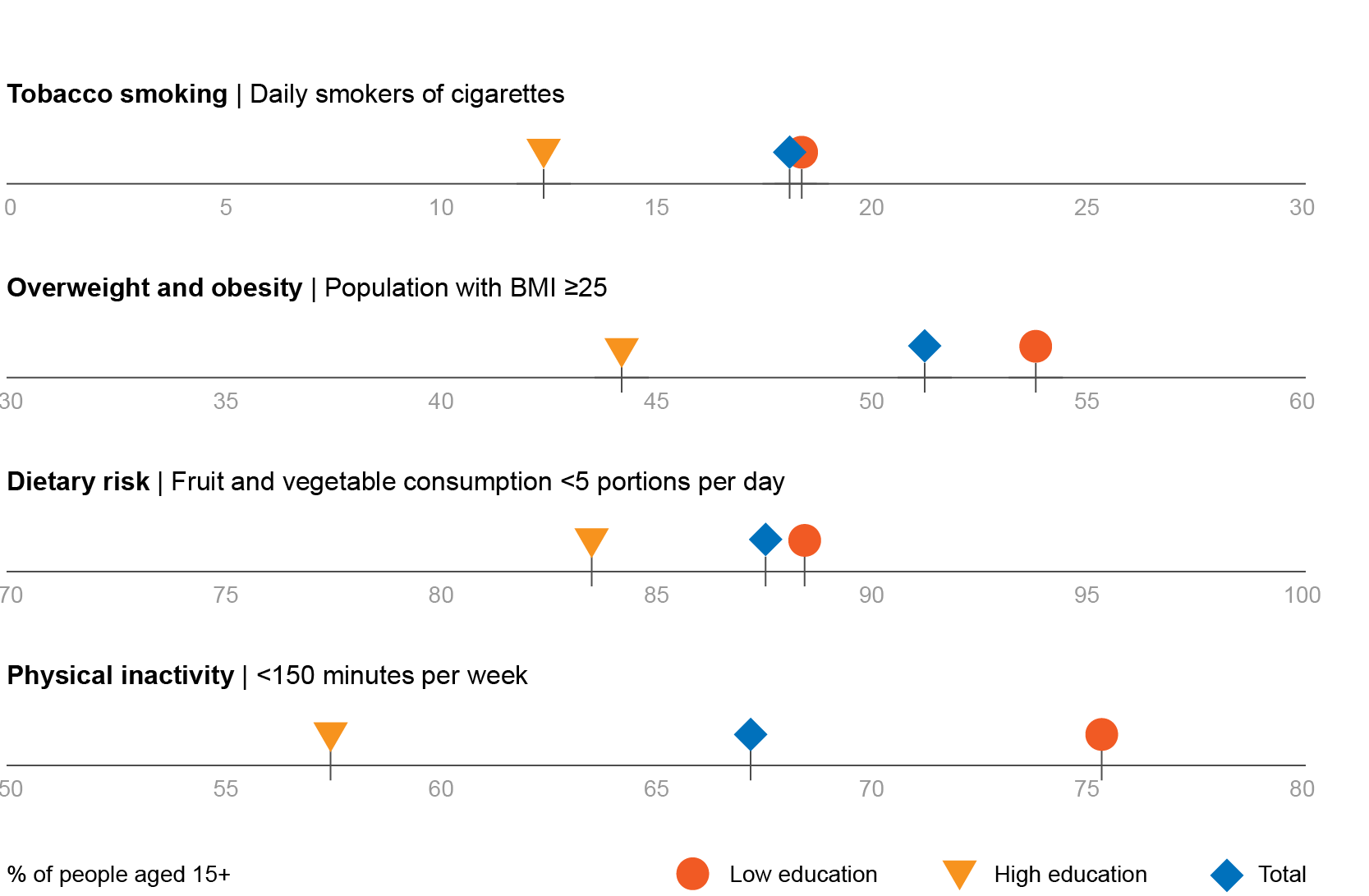
Strong inequalities persist in exposure to risk factors, particularly affecting those from lower socioeconomic backgrounds; for example, daily smoking is nearly 50% more prevalent among people with lower education and levels of overweight and obesity are 21% higher. Similarly, both the consumption of fruits and vegetable and the levels of physical activity are lower.
Socio economic gaps to the detriment of people with lower education levels are found for several cancer risk factors.
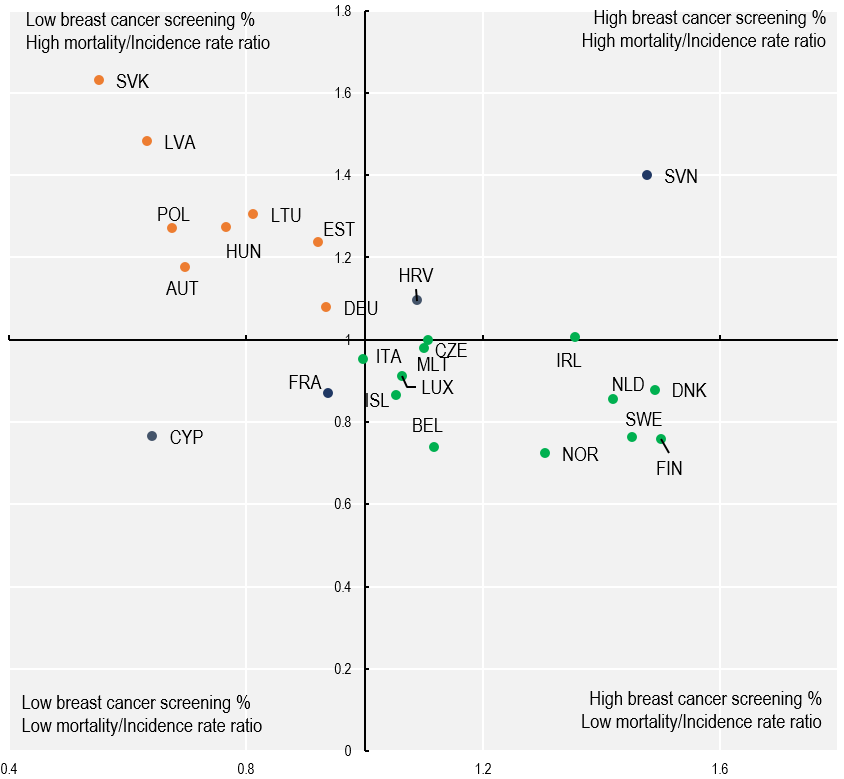
Assessing and improving cancer care from prevention to treatment is essential for promoting longer, healthier lives. For instance, cancer screening is associated with better cancer outcomes. When looking at breast cancer screening, rates vary nine fold across countries in the EU, with an EU27 average of 54%, and countries with higher participation rates in breast cancer screening had a lower ratio of breast cancer mortality to incidence rate.
Higher participation rates in breast cancer screening programmes are associated with lower ratios of breast cancer mortality to incidence.
There are large differences across countries as concerns the public reimbursement of new cancer medicines. For example, Germany reports that coverage is available for all cancer medications with EMA marketing authorisation, while in Malta, Cyprus and Latvia less than a third are reimbursed or publicly covered.
There is marked variability in coverage of oncology medications across countries.
Shares of selected indications of cancer medicines with EMA marketing authorisation that received public reimbursement/coverage
Overall, this report highlights the need to invest in comprehensive and inclusive cancer prevention and control policies – with particular emphasis on disadvantaged groups. It provides policy makers with fiscal, regulatory and health systems organisation tools, as well as examples of initiatives that can be undertaken in primary care, workplaces, and schools to better control cancer and counter inequalities.
Downloads
-
DownloadБългарски
-
DownloadEspañol
-
DownloadČeština
-
DownloadDansk
-
DownloadDeutsch
-
DownloadEesti
-
DownloadΕλληνικά
-
DownloadFrançais
-
DownloadHrvastki
-
DownloadItaliano
-
DownloadLietuvių
-
DownloadLatviešu
-
DownloadMagyar
-
DownloadNederlands
-
DownloadPolski
-
DownloadPortuguês
-
DownloadRomână
-
DownloadSlovenský
-
DownloadSlovenščina
-
DownloadSuomi
-
DownloadSvenska
-
DownloadÍslenska
-
DownloadNorsk
- Looking for another language which is not on the list? Find out why.
